Introduction: Relapse remains a significant challenge in the management of high-risk B-cell acute lymphoblastic leukemia (B-ALL) patients undergoing allogeneic hematopoietic stem cell transplantation (allo-HSCT). Existing post-transplant relapse prevention strategies for high-risk B-ALL patients after transplantation, particularly in cases of Philadelphia chromosome-negative B-ALL, have limitations and suboptimal efficacy. This study aims to evaluate the efficacy and safety profile of prophylactic or preemptive infusion of donor-derived CD19 chimeric antigen receptor T (CAR-T) cells in high-risk B-ALL patients after allo-HSCT.
Methods: Between May 2017 and July 2022, high-risk B-ALL patients with minimal residual disease (MRD) positive or MRD negative status after allo-HSCT were enrolled in clinical trials of donor-derived CD19 CAR-T cell therapy (ChiCTR 2000041025 and ChiCTR-ONN-16009862). The primary outcome was the cumulative incidence of relapse (CIR). Secondary outcomes were progression-free survival (PFS), overall survival (OS) and CAR-T cell treatment-related toxicities.
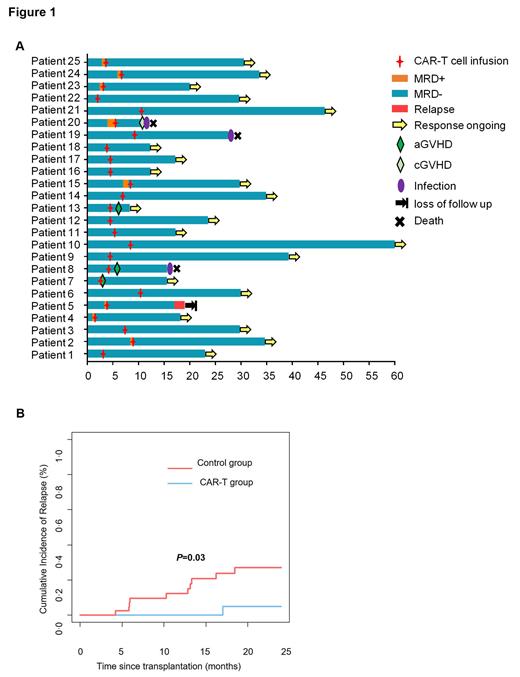
Results: A total of 25 high-risk B-ALL patients who received infusion of donor-derived CD19 CAR-T cells after allo-HSCT were enrolled in the CAR-T cell group, including 8 patients with MRD and 17 patients without MRD. A contemporaneous cohort of 43 high-risk B-ALL patients who did not receive CAR-T cell therapy in MRD-positive or MRD-negative status after transplantation was also included as a control group. The median age of patients enrolled in the CAR-T group was 29 years (range: 9-60 years). The median infused CAR-T cell dose was 2.5×10^6/kg (range: 1.0-5.0×10^6/kg), with a median time from transplantation to CAR-T cell treatment of 122 days (range: 45-315 days). The median follow-up duration was 23.6 months (range: 8.3-60.6 months). Of the 25 patients in CAR-T group, eight MRD-positive patients achieved MRD-negative remission after CAR-T cells treatment (Figure1A). The two-year cumulative incidence of relapse in the CAR-T cell group was significantly lower at 4.8% (95% CI: 0.0%-12.6%) compared to the control group's incidence of 26.6% (95% CI: 11.4%-41.8%, P = 0.03,Figure1B). Additionally, the CAR-T cell group exhibited a higher two-year PFS rate [86.3% (95% CI: 71.8%-100%)] compared to the control group [63.5% (95% CI: 48.0%-79.0%), P = 0.04]. However, the two-year OS rates were comparable between the CAR-T cell group [91.0% (95% CI: 79.0%-100%)] and the control group [79.1% (95% CI: 66.0%-92.2%), P = 0.20]. Adverse events were well tolerated, and no patients experienced grade 3-4 cytokine release syndrome or any grade of immune effector cell-associated neurotoxicity syndrome. Hematological cytopenia was the most severe CAR-T cell related toxicity, but the toxicity was manageable, and only three patients experienced acute graft-versus-host disease following CAR-T cell infusion.
Conclusions: Prophylactic or preemptive infusion of CAR-T cells after allo-HSCT demonstrated a reduced incidence of relapse and acceptable adverse events in high-risk B-ALL patients. These findings highlight the potential of CAR-T cell therapy as a promising strategy for relapse prevention in high-risk B-ALL patients after allo-HSCT.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal